Magnitude of Tuberculosis in the Philippines
Tuberculosis or TB is an infectious disease caused by the bacteria called Mycobacterium tuberculosis. It is transmitted from a TB patient to another person through coughing, sneezing and spitting. Thus, close contacts, especially household members, could be infected with TB. Lungs are commonly affected but it could also affect other organs such as the kidney, bones, liver, and others. TB is curable and preventable. However, incomplete or irregular treatment may lead to drug-resistant TB or even death.Tuberculosis is a major public health problem in the Philippines. In 2010, TB was the 6th leading cause of mortality with a rate of 26.3 deaths for every 100,000 population and accounts for 5.1% of total deaths. This is slightly lower than the five-year average of 28.6 deaths per 100,000 population. More males died (17,103) compared to females (7,611).
The country had conducted three National TB Prevalence Survey (NTPS) that describe the magnitude and the trend of the TB problem. The results were as follows:
| Indicators | NTPS 1983 | NTPS 1997 | NTPS 2007 |
| Prevalence of culture-positive TB | 6.6/ 1,000 | 3.1/ 1,000 | 2.0/ 1,000 |
| Prevalence of sputum smear-positive TB | 4.2% | 4.2% | 6.3% |
| Prevalence of those with CXR findings suggestive of TB | 2.5% | 2.3% | 2.1% |
| Rate of TB symptomatic | 17.0% | 18.4% | 13.5% |
| Prevalence of those with CXR findings suggestive of TB | 8.6/ 1,000 | 3.1/ 1,000 | 4.7/ 1,000 |
Prevalence of those with CXR findings suggestive of TB 8.6/1,000 3.1/1,000 4.7/1,000 TB is more prevalent among males compared to females and among the 25-55 year old age group. It is also higher among the malnourished and diabetics. The 1997 survey showed that prevalence of TB among the urban poor in Metro Manila is twice that of the general population. The first national Drug Resistance Survey was done in 2003-2004 and revealed the following prevalence of drug resistance: 4% among the new cases, 21% among the re-treatment cases, and 5.7% combined. The second National Drug Resistance Survey was done in 2011-2012 and showed a decrease in the prevalence of drug resistance among new cases from 4% to 2%. However, there was no change in the prevalence of drug resistance re-treatment cases which remained at 21%.
We need to end TB from this planet by 2030. Yet, the Philippines is among the few countries where the number of people with TB continues to increase every year.
The Philippines must rise to this challenge and deliver on the commitments that Secretary Duque made in New York. For that, the country needs to run an aggressive and sustained campaign against TB. That is the only way to bend the epidemic curve of TB towards its elimination.
It’s time to ask ourselves some hard questions
Fighting TB requires us to go beyond the health sector. Are we engaging other departments enough to act and be accountable for their roles in ending TB? For instance, about 100,000-150,000 people with TB suffer from catastrophic costs while seeking treatment in the public sector every year. The main reasons for that are loss of income, transport costs and nutritional supplements. Can the Department of Social Welfare and Development support patients using conditional cash transfers for screening, testing and treatment against TB?Fighting TB requires the private and public sectors to work together. Are the both sectors collaborating with each other enough? About 150,000 people with TB seek care in the private sector every year although most of them are poor. They may do that because of time, distance and confidentiality issues in public health facilities. They have the right to choose their providers. But unless we support those patients too, we can never achieve the national targets to end TB. Besides, these patients are more likely to suffer from catastrophic costs due to TB care than those who seek care in the public sector. Can the Department of Health provide advanced diagnostics and drugs for free to these patients within the private sector networks without compelling them to change their providers?
Fighting TB requires systematic screening for TB among all high risk groups, especially in vulnerable communities. Are we doing that enough already? According to the bold and ambitious national strategic plan of the Department of Health, about 6-9% of the general population needs to undergo chest X-ray screening annually. Similarly, 2-3% of the general population needs to undergo testing with rapid molecular diagnostics annually. Has the Department of Health been able to mobilize adequate quantities of the required diagnostics and drugs to ensure their uninterrupted supply?
Fighting TB using an aggressive and sustained campaign requires adequate boots on the ground. Do we have enough of them already? Ideally, the cities and municipalities that have the highest number of missing patients should have dedicated frontline supervisors to coordinate and run the TB campaign. Additionally, all big hospitals should have dedicated officers to coordinate and implement screen-all policy against TB within those hospitals. This will help to find people with TB early and treat them promptly, thereby cutting the chain of transmission rapidly. Can the local governments deploy such frontline supervisors and workers quickly?
As a nation, it’s time to answer these questions and act!
Ending TB requires concerted action by all sectors and all care providers. Everyone has a role to play in ending TB – individuals, communities, businesses, governments, societies. Everyone must join the race to end TB by 2030. Can all readers of this article post their ideas on social media using the hashtag of #RaceToEndTB? Can all readers also reach out to their local governments to advocate for adequate financial and human resources to screen all high risk groups with chest X-ray annually and for TB symptoms regularly?In New York, Secretary Duque declared that he will focus on three game-changers: high level commitment, massive screening, testing and treatment, and mandatory notifications by the private sector. He has appealed to all of us to lend our full support to the Department of Health. Are we ready to join him in this now-or-never fight to end TB once and for all?
The World Health Organization is committed to working side-by-side with the communities, the governments and other partner agencies to wipe out this top killer. The clock is ticking. We cannot lose another day. It’s time to ensure that no one dies of TB anymore. It’s time to find and treat the 2.5 million Filipinos with TB by 2022. It’s time to #EndTB!
Decline in reported TB cases an effect of the COVID-19 pandemic
The Department of Health (DOH) reported that although the number of tuberculosis (TB) cases reported in the country in the first three months of 2020 has drastically gone down, this does not necessarily mean good news.From January to March this year, the National Tuberculosis Control Program (NTP) of the DOH recorded a total of 88,662 new and relapse TB cases, declining steeply by almost 20% between February (30,728) and March (24,782).
“We see this as a direct effect of the COVID-19 pandemic on a critical disease prevention and control program like TB,” said Health Secretary Francisco T. Duque III. “The quarantine has extremely affected and limited the health seeking behaviors of our fellow Filipinos,” he added.
According to Duque, unlike other health programs, having fewer cases is not an indicator of success for the TB program. “Our goal for our TB program is to find and treat as many TB cases as possible. Only by finding and treating these cases can we limit its spread and achieve our dream of a TB-free Philippines.”
In recent years, the DOH has boosted its active case finding initiatives, organizing community outreach activities and setting up local TB task forces for community surveillance. From 2017-2019, the DOH reached, on the average, 93% of its annual target of notified cases. But the COVID-19 quarantine has restricted such interventions to find, test, treat and prevent TB cases in hospitals, health facilities and communities.
Following this, on March 16, 2020 the DOH-NTP issued Department Memorandum 2020-0128 entitled “Ensuring Continuous TB Services During Community Quarantine” to provide guidance and ensure safety of both the facility staff and patients, who are at high risk of infection. The following guidelines are also recommended for the implementation of the different screening activities and surveillance:
Screening of Presumptive TB, through passive, active, intensified, or enhanced case finding, shall continue subject to mandated social distancing and usual infection control procedures. Avoid gathering people in one place for TB screening and provide masks for healthcare staff and patients. Usual contact tracing efforts are still to be implemented with strict compliance on infection control measures. Reporting or notification of cases are still through the Integrated TB Information System(ITIS). Soon after the General Community Quarantine was imposed in Metro Manila and other parts of the country, the DOH also issued an administrative order to ensure continuous TB services. Patients who are currently enrolled for TB treatment in government facilities are advised to secure their one-month supply of anti-TB medicines.
“We are taking unprecedented steps to treat our fellow Filipinos with active TB disease. We are monitoring our stocks to make sure those with active TB have access to free medicines and are able to complete their treatment regimen,” said Duque.
The DOH through the NTP is continuously working to ensure uninterrupted TB services during community quarantine and is closely collaborating with its key partners to mitigate the effects of COVID-19 through various initiatives and innovations.
TB Patients are encouraged to establish a close coordination with their health providers during the pandemic. Likewise, health care providers are also mandated to call and follow up with patients every 1-2 weeks to check for any problems or adverse reactions that the patient may experience.
In 2019, the Philippines had the highest TB incidence in Asia with 554 cases per 100,000 people, according to a World Health Organization (WHO) report. Approximately, 74 Filipinos die of TB every day and is among the top 10 causes of death in the country.
In September 2018, Duque committed to find and treat 2.5 million Filipinos with TB at the United Nations High Level Meeting on TB in New York City. Since then, the DOH has recorded
1.1 million TB cases, leaving 1.4 million more cases to find and treat in the next 2.5 years.
Using a projection modeling based on a recent study of the global Stop-TB Partnership, DOH estimates that, because of the pandemic, notified cases in 2020 will only reach 72% of the annual target. By the end of 2022, if this trend continues, the Philippines will miss its commitment by almost 300,000 cases.
“One TB case that we fail to find and treat may spread the infection to at least 10 other people. The reservoir of undetected TB cases will further increase,” said the Health Chief.


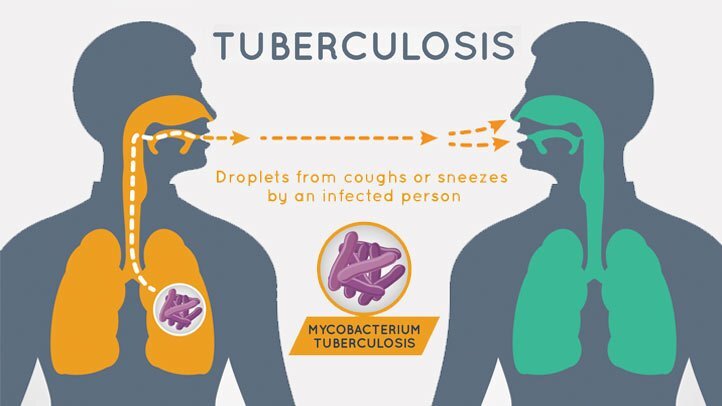 Infection path
Infection path Cutaneous tuberculosis lesions on a child's face. Tuberculosis (TB) is a disease caused by infection by the bacterium Mycobacterium tuberculosis. In most cases it affects the lungs (pulmonary tuberculosis), which is generally fatal if untreated. In some cases it affects the skin, causing a rash. This form of the disease can cause ulceration and destruction of underlying tissues
Cutaneous tuberculosis lesions on a child's face. Tuberculosis (TB) is a disease caused by infection by the bacterium Mycobacterium tuberculosis. In most cases it affects the lungs (pulmonary tuberculosis), which is generally fatal if untreated. In some cases it affects the skin, causing a rash. This form of the disease can cause ulceration and destruction of underlying tissues
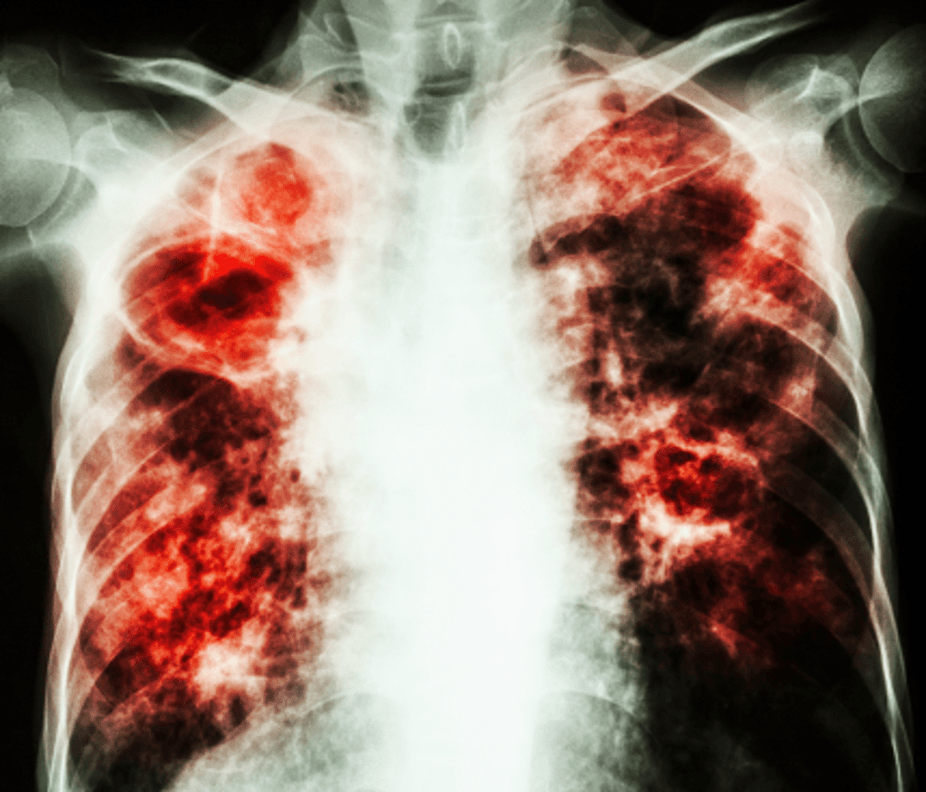 Post-primary cavitating tuberculosis. False-colour Chest X-ray showing extensive fibrosis in both lungs (red areas), the consequences of primary pulmonary tuberculosis. In most chest diseases, including tuberculosis, the appearance on X-rays mirrors the pathology. The primary tuberculous infection, due to the bacterium Mycobacterium tuberculosis, results in areas of pneumonitis (inflammation). In the post-primary stage cavitation may occur, followed by progressive fibrosis.
Post-primary cavitating tuberculosis. False-colour Chest X-ray showing extensive fibrosis in both lungs (red areas), the consequences of primary pulmonary tuberculosis. In most chest diseases, including tuberculosis, the appearance on X-rays mirrors the pathology. The primary tuberculous infection, due to the bacterium Mycobacterium tuberculosis, results in areas of pneumonitis (inflammation). In the post-primary stage cavitation may occur, followed by progressive fibrosis. Tuberculosis in childhood,
Tuberculosis in childhood,