It is estimated that more than 30 percent of adults or about 1 in 3 to 4 adults have high blood pressure or arterial hypertension. This percentage is constantly increasing.
More and more people are said to suffer from elevated blood pressure. A quarter to half of them would not know that their blood pressure is too high. In most cases, elevated blood pressure has to do with a combination of hereditary factors and lifestyle. The older one gets, the higher the chance of high blood pressure. Arterial hypertension is a major risk factor for cardiovascular disease, especially stroke (CVA) and myocardial infarction. Especially if you also have other risk factors, such as high cholesterol, overweight or if you smoke. Other organs can also be affected, such as the kidneys. Those complications usually develop over a period of several years. High blood pressure rarely causes complaints. It is therefore important that you have your blood pressure measured at every doctor's visit. It happens all too often that hypertension is detected when a complication starts to lead to symptoms, but by then it is already too late to prevent those complications. Therefore, hypertension is sometimes called the "silent killer".
What is blood pressure?
 With each heartbeat, the heart contracts and blood is pumped from the left ventricle into the arteries of the large circulatory system (systemic circulation). This blood exerts pressure on the artery wall: this is arterial pressure or blood pressure.
With each heartbeat, the heart contracts and blood is pumped from the left ventricle into the arteries of the large circulatory system (systemic circulation). This blood exerts pressure on the artery wall: this is arterial pressure or blood pressure.
- Systolic blood pressure or upper pressure: the first digit, the highest, when the heart contracts and blood flows out
- Diastolic blood pressure or negative pressure:the second digit, the lowest, when the heart relaxes and is filled with blood. Arterial blood pressure is expressed in millimeters of mercury, for example 120/80 mm Hg (or 12/8).
Arterial blood pressure can vary depending on the time of day, from one day to the next and under the influence of emotions, stress, physical activity, and so on. For example, the pressure is higher when we are awake during the day and lower when we sleep. It is also higher during physical exertion than when you sit quietly.
When is your blood pressure too high (hypertension)?
- One speaks of high blood pressure or arterial hypertension when the blood pressure values are on average higher than 140 mmHg systolic and / or 90 mmHg diastolic (140/90 or 14/9).
- For persons aged 60 years and older without diabetes, familial hypercholesterolemia or manifest cardiovascular disease, systolic blood pressure = 160 mmHg is considered elevated.
- With a systolic blood pressure of more than 180 mmHg and /or a diastolic blood pressure of more than 110 mmHG, one speaks of a serious hypertension.
- In some people, especially those over 60, isolated systolic hypertension occurs. This is the case when systolic blood pressure is higher than 140 mmHg and diastolic pressure is below 90 mmHg. This is also an important risk factor for cardiovascular disease.
| Systolic blood pressure (mmHg) | Diastolic blood pressure (mmHg) | ||
| Optimal | < 120 | and> | < 80 |
| Normal | 120 – 129 | and/or | 80 – 84 |
| Normally high | 130 – 139 | and/or | 85 – 89 |
| Hypertension grade 1 | 140 – 159 | and/or | 90 – 99 |
| Hypertension grade 2 | 160 – 179 | and/or | 100 – 109 |
| Hypertension grade 3 | ≥ 180 | and/or | ≥ 110 |
| Isolated systolic hypertension | ≥ 140 | and | < 90 |
How is blood pressure measured?
The only way to detect high blood pressure in time is to measure your blood pressure regularly.
Because blood pressure can fluctuate (slightly) during the day and from day to day, and is also influenced by external factors (strong emotions, exercise, temperature, alcohol consumption, meals...) the blood pressure must be measured several times to determine whether or not you have an elevated blood pressure.
Classic measurement of blood pressure by the doctor
The classic blood pressure measurement is done by a doctor during a consultation or a home visit. The diagnosis of hypertension is based on different measurements, during the same consultation and during several consultations.
- To be able to diagnose high blood pressure, at least two measurements are needed, spread over time.
- The measurement is done in a sitting position in a calm and quiet environment, after a few minutes of rest and with an interval of 1 to 2 minutes. The blood pressure can also be measured in a supine position. In elderly patients, diabetics and people who suffer from dizziness when they suddenly stand upright or who are in danger of falling when they stand up (which can happen when they take certain medicines), it is recommended to measure blood pressure again after 1 and 5 minutes in a standing position.
- In the first examination, blood pressure is measured on both arms; if the values differ from each other, the reference shall be that of the arm with the highest value. The heart rate is measured after the second measurement of blood pressure, in a sitting position and for at least 30 seconds.
- In some people, the blood pressure measured by the doctor is higher than the normal blood pressure ('white coat hypertension'). Therefore, it can be useful to measure blood pressure at home without the doctor being present. The reverse also occurs: when your doctor measures your blood pressure, it is normal, but once back home it rises again. That phenomenon is called masked hypertension. It can also be useful to measure blood pressure at home.
In this examination, you will receive an arm cuff in the hospital that is connected to a device that both registers and pumps (to inflate the cuff), and that is worn on a band around the abdomen. Blood pressure is measured at intervals for 24 hours, for example every 20 minutes. After 24 hours, the device must be returned to the hospital.
This technique has the great advantage that the doctor has many measurement values and that the measurements are carried out in the natural environment during normal daily activities.
Currently, the 24-hour outpatient measurement is the most reliable study to obtain certainty whether a person's blood pressure is too high, and to check whether the medicines for high blood pressure work sufficiently.
- Unusual fluctuations in blood pressure with various measurements by the doctor.
- An important difference between the measurement by the doctor and the home blood pressure measurement.
- High blood pressure in people at low risk for cardiovascular disease.
- High blood pressure that is not controlled with medicines ('resisting hypertension').
- Symptoms that indicate periods of blood pressure drop, especially in the elderly and in people with diabetes.
The blood pressure values at home measurement or 24-hour outpatient measurement are usually slightly lower than a blood pressure measurement that a doctor performs. This is why the threshold values for high blood pressure differ according to the method of measurement:
Measurement by the doctor: =140 and/or = 90
Home blood pressure measurement: = 135 and/or = 85
Ambulatory 24-hour blood pressure measurement: = 130 and/or = 80
Causes of high blood pressure
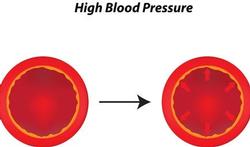
 Increased blood pressure is due to the loss of elasticity of the large arteries.
Increased blood pressure is due to the loss of elasticity of the large arteries.
Primary or essential hypertension
Usually there is no exact cause for the high blood pressure. One then speaks of primary or essential hypertension.
The origin of hypertension is the interplay between genetic factors (the risk of developing hypertension is greater in someone who has parents with hypertension) and environmental factors (lifestyle) such as obesity, a sedentary life, excessive use of salt, and excessive alcohol consumption.
Chronic stress may play a role, but this hasn't really been demonstrated. Stress is a risk factor for cardiovascular disease.
Secondary hypertension
In about 1 in 10 cases, hypertension is a result of another condition. This is called secondary hypertension. The higher the blood pressure, and the younger you are if you get high blood pressure, the higher the chance that it is secondary hypertension.
- Kidney disease: Practically all kidney diseases can cause arterial hypertension, such as a narrowed renal artery (renovascular hypertension).
- Excessive production of certain hormones by the adrenal glands: aldosterone (primary hyperaldosteronism or Conn disease), catecholamines such as norepinephrine and adrenaline (pheochromocytoma), corticosteroids (Cushing's disease).
- Hypothyroidism: when the thyroid gland produces too few thyroid hormones.
- Obstructive sleep apnea: repeated and more or less long episodes of respiratory arrest during sleep, often combined with snoring and daytime sleepiness.
The (long-term) use of certain medicines, including: - some anti-inflammatories including aspirin or acetylsalicylic acid),
- corticosteroids
- sympathomimetics (decongestants, sibutramine, cocaine),
- stimulants such as amphetamine
- erythropoietin (EPO),
- slimming pills...
- The contraceptive pill usually hardly causes an increase in blood pressure and it is very rare for a young woman to get hypertension because of the pill. However, it is useful to have blood pressure measured before starting the contraceptive pill.
- In children or adolescents, other causes may be at the root of high blood pressure, such as a narrowing of the aorta. In pregnant women, gestational hypertension and preeclampsia may occur.
Who is at increased risk of high blood pressure?
n most cases, elevated blood pressure has to do with a combination of hereditary factors and environmental factors.
- Heredity
If one of your parents suffers from hypertension, you have an increased risk of also getting high blood pressure.
But the moment when hypertension develops can be delayed and even avoided by a healthy lifestyle and sensible eating habits. - Age
The likelihood of hypertension increases with age. Up to the age of 30, only 1 to 2% of the population has high blood pressure, with the over-60s rising to around 60%. In particular, systolic blood pressure continues to rise, while diastolic blood pressure from the age of 60 tends to fall again. It is believed that there is about a 5% increase in elevated blood pressure every ten years in people over 65. From the age of 80, blood pressure decreases again.
The occurrence of isolated systolic hypertension also increases with age, from approximately 5% at the age of sixty to 30% at the age of eighty. - Gender
Hypertension is slightly more common in men than in women. Women are often affected by hypertension after menopause. Over the age of 60, there are more women than men with hypertension. - Lifestyle
- Obesity: Overweight (BMI >25) and in particular an increased lumbar/hip ratio (102 centimeters or more for men, 88 centimeters or more for women) is a major risk factor.
- A sedentary life;
- Excessive salt and alcohol consumption;
Stress: elevated blood pressure is more common in people with chronic stress, but the exact mechanism is not clear. This also applies to the link between high blood pressure and exposure to noise. Stress is certainly a risk factor for cardiovascular disease.
- Smoking: probably does not affect the blood pressure itself, but it does increase the risk of cardiovascular disease.
Can you avoid high blood pressure?
The onset of elevated blood pressure can be delayed and even largely prevented by a healthy lifestyle.
- Avoid overweight
Overweight (a BMI above 25 kg) is a major risk factor for the development of elevated blood pressure. In risk groups with normal blood pressure, it was shown that by losing a few kilos they had significantly less to do with elevated blood pressure. Or at least this slows down its development.
The goal is to maintain a normal weight, i.e. a Body Mass Index (BMI) of less than 25. In the elderly, the relationship between BMI and health is not so clear-cut and a BMI = 30 is acceptable.
A weight reduction of 3 to 9% of total body weight results in both systolic and diastolic blood pressure reduction of approximately 3 mmHg. - Smoking cessation
By smoking a cigarette, blood pressure rises for about 15 minutes. In the long term, smoking has not been proven to cause increased blood pressure. But smoking is a very important risk factor for cardiovascular disease. Smoking cessation is therefore essential. If you continue to smoke, the beneficial effect of any drug treatment will never be optimal. - Use less salt
Although there are still many discussions about the relationship between salt and high blood pressure, it is recommended to consume a maximum of 5 to 6 g of salt per day. The average salt consumption now fluctuates around 9 to 10 g per day. Keep in mind that many foods already contain salt. For example, an ordinary large loaf of bread already contains 4 g of salt. Stock cubes and prepared meats can also contain a lot of salt.
You can use less salt by not adding salt to the food and using prepared dishes (soups, sauces...) sparingly. - Drink less alcohol
Alcohol consumption is a major risk factor for high blood pressure. Drinking alcohol increases blood pressure, whether it is moderate and regular alcohol consumption or significant and high alcohol consumption ("binge drinking"). On the other hand, moderate daily use of a maximum of two to three 'standard drinks' for men and one to two for women could potentially reduce the risk, but there is still a lot of discussion about this. It is certainly no reason to drink a few glasses every day. - Eat healthy
Research has shown that the so-called "DASH" diet (Dietary Approaches to Stop Hypertension) lowers blood pressure in people with normal blood pressure as well as in people with elevated blood pressure. This diet is based on eating a lot of fruits, vegetables, cereal products and nuts, little saturated fats (such as butter, whole milk, fatty meats and fatty cheese) and more unsaturated fats (vegetable fats and fish). The combination with a low-salt diet has an additional blood pressure lowering effect. - Exercise more Regular exercise lowers blood pressure: walking, walking, cycling for at least 30 minutes a day... If you are over 40 years old and/or lead a sedentary life, consult your doctor whether you are fit enough to exercise and which sports are most suitable. Do not exaggerate at first, but gradually build up the duration and intensity of the exercise activities.
What are the symptoms of high blood pressure?
High blood pressure rarely causes complaints. Sometimes high blood pressure is accompanied by headaches, ringing in the ears, dizziness, fatigue, spots or flies in front of the eyes, nosebleeds, shortness of breath... But usually it is discovered by chance, for example, when visiting the doctor for something else. It is therefore important that you have your blood pressure measured at every doctor's visit. All too often, hypertension is detected when organ damage has already occurred, but by then it is already too late to prevent those complications. Therefore, hypertension is sometimes called the "silent killer".
How often should you measure your blood pressure?

- You have no known risk factors for cardiovascular disease
- Have your blood pressure (and other risk factors for cardiovascular disease such as high cholesterol) measured every five years.
- If you are between 40 and 80 years old, a blood pressure measurement is recommended every time you consult your (family) doctor for a different reason.
- Also have your blood pressure measured:
- when you use hormonal contraception for the first time
- if you suspect migraines
- when you are pregnant.
- In case of risk factors for cardiovascular disease, it is recommended to have your blood pressure measured at least once a year (or more if your doctor deems it necessary):
- you have cardiovascular disease
- you have high cholesterol or this runs in your immediate family
- you are being or have been treated for high blood pressure in the past.
- you have diabetes
- you have kidney disease
- you have rheumatoid arthritis
- you are over 50 and smoke.
Why is high blood pressure dangerous?
High blood pressure is not a disease, but long-term high blood pressure is a major risk factor for cardiovascular disease, especially stroke (CVA) and myocardial infarction. Other organs such as the kidneys and eyes can also be affected. Those complications usually develop over a period of several years.
Hypertension is considered the second cause of premature death in the West, after smoking, and the leading cause of death from cardiovascular disease. Cardiovascular diseases are responsible for 45% of deaths in Belgium.
Hypertension plays a role in half of all cardiovascular diseases.
• The risk of complications is almost proportional to blood pressure: the higher the blood pressure, the greater the risk. Research shows that the risk of complications starts with a blood pressure of 115/75 mmHg and that this doubles with every increase of 20/10 mmHg.
• The risk of cardiovascular disease depends not only on blood pressure, but also on whether other risk factors are involved, such as diabetes, smoking and high cholesterol.
For example, a non-smoker aged 58 years with a systolic pressure of 155 mmHg and a cholesterol level of 170 mg/dl is 4% at risk of dying from cardiovascular disease within ten years. At the same blood pressure (155 mmHg), the risk increases by 17% in this 58-year-old man if he smokes and if his cholesterol level is 280 mg/dl.
• Treatment of high blood pressure reduces the risk of mortality by about 10%, heart disease by about 15%, stroke by about 30%.
The heart
High blood pressure can cause damage to the walls of your arteries. This can cause the arteries to become clogged. As a result, your heart has to work harder and harder to pump the blood around, which can thicken the heart wall. This causes all kinds of complications such as pain in the chest during exercise and heart clamping (angina pectoris), a heart attack and heart failure.
The risk of heart damage also depends on other risk factors such as smoking, obesity, high cholesterol, diabetes and so on.
The brain
An artery that feeds the brain can become clogged by a blood clot (brain thrombosis) or it can burst and cause a brain hemorrhage. In both cases, one speaks of a stroke or stroke, which can result in paralysis, a coma or the death of the patient.
The kidneys
If the arteries that feed the kidneys become clogged, renal insufficiency develops, which will sometimes require treatment with an artificial kidney (dialysis) or a kidney transplant. That is why it is important that the kidneys are examined regularly if you have high blood pressure.
The large blood vessels
The large blood vessels can clog, causing pain when walking (intermittent claudication or shop window legs). Complete closure of a leg artery can lead to gangrene if not treated in time. They can also expand, which can give rise to life-threatening bleeding.
Eyes
High blood pressure can damage the blood vessels in the eye over time, which can cause abnormalities of the retinal (retinal retinopathy).
What is a hypertensive crisis (malignant hypertension) A hypertensive crisis or a malignant hypertension is a sharp increase in blood pressure (usually > 120 to 130 mmHg diastolic and > 200 to 220 mmHg systolic). This can be accompanied by acute damage to the brain, heart, kidneys, large blood vessels or eyes.
- In the event of a hypertensive crisis with organ damage or neurological symptoms, you should be admitted to a hospital as soon as possible and receive antihypertensive drugs via an infusion.
- In case of hypertensive crisis without organ damage, oral treatment is initiated or increased.
Additional studies in high blood pressure
When high blood pressure is detected, additional examinations are usually needed to determine:
- whether certain organs (e.g. kidneys, heart, eyes...) are already damaged
- whether other risk factors for cardiovascular disease (e.g. high cholesterol, diabetes, etc.) are present
- whether there are other causes of high blood pressure (secondary hypertension), for example kidney disease, adrenal gland disease, obstructive apnea syndrome...
Depending on the severity of the high blood pressure and additional risk factors, the following tests may be required. If necessary, your doctor will refer you to the hospital for this.
- Blood and urine tests for the storage of o.m. elevated cholesterol, kidney damage, diabetes...
- Electrocardiogram: this allows a thickening of the heart muscle to be detected (hypertrophy left ventricle), which is the result of a serious hypertension, whether or not longer existing.
- Ultrasound of the heart, carotid arteries and kidneys.
- Measurement of blood pressure on arms and legs, allowing one to calculate the ankle-arm index to detect an artery narrowing in the lower limbs.
- Eye fundus examination to detect any damage to the retina and/or optic nerve.
- A scan of the adrenal glands
When should high blood pressure be treated?
 Whether and how high blood pressure should be treated depends not only on blood pressure levels, but also on the risk of cardiovascular disease and the presence of organ damage (e.g. kidney damage, thickening of the heart wall...).
Whether and how high blood pressure should be treated depends not only on blood pressure levels, but also on the risk of cardiovascular disease and the presence of organ damage (e.g. kidney damage, thickening of the heart wall...).
Usually, the treatment will also focus not only on the increased blood pressure, but also on the other risk factors, such as smoking, obesity, diabetes, lack of exercise...
Treatment with antihypertensive medicines is recommended:
- Persons without other risk factors for cardiovascular disease and without organ damage:
- Very severe hypertension grade 3 (=180 and/or =110 mmHg): immediate treatment.
- Severe hypertension grade 2 = 160 and/or = 100 mmHg): treatment with drugs if non-drug lifestyle adjustments after 3 months have insufficient effect on blood pressure.
- Persons at risk of cardiovascular disease or organ damage
In persons with organ damage or an increased risk of cardiovascular disease, treatment is started at a blood pressure of = 140 and / or = 90 mmHg.
Whether treatment with blood pressure-lowering drugs is necessary depends mainly on your risk of cardiovascular disease. That is why your doctor will draw up a global risk profile based on the European SCORE table.
The overall cardiovascular risk is the risk of developing a cardiovascular accident (infarction, stroke, etc.) over the next ten years. This risk is influenced by all the risk factors and damage to the heart and blood vessels, and not just by increased blood pressure. According to the SCORE tables, a risk of death within ten years due to cardiovascular disease of 5% or more is considered high.
In addition to risk factors, the overall cardiovascular risk is also influenced by damage to the heart (thickening of the heart muscle or hypertrophy of the left ventricle), kidney damage (proteins in the urine, poor functioning of the kidneys) or vascular diseases (heart or cerebral infarction). - Persons with a greatly increased risk of cardiovascular disease
Always treatment with blood pressure lowering drugs + lifestyle adjustment- a SCORE risk >10%
- patients with previous cardiovascular problems, such as a heart or cerebral infarction (CVA) or a TIA (a transient ischemic attack is a transient period of neurological failure, which can last from a few minutes to several hours. A TIA is a major risk factor for developing a stroke)
- individuals with diabetes
- Patients with organ damage to the heart, kidneys, eyes...
- 4. Individuals at moderate risk of cardiovascular disease (SCORE risk between 5 and 10%)
Usually lifestyle measures + possibly after a few months blood pressure lowering medicines if the lifestyle changes are not sufficient.
Treatment depends on the number of additional risk factors, such as:- a family history of heart disease
- obisity
- lack of exercice
- rheumatoid arthritis
- impaired kidney function
- excessive alcohol consumption
- Individuals at low risk of heart disease (SCORE risk of les than 5%)
Especially lifestyle adjustment, only treat medically at very high blood pressure values.
Purpose of treatment
The aim of the treatment is of course to lower blood pressure, but also and especially to prevent or limit the risk of cardiovascular disease and damage to other organs.
- The aim is to reduce blood pressure to less than 140 and 90 mmHg on average.
- In people with diabetes or kidney disease, the target is a blood pressure of 130/85 or 125/75 mmHg, depending on the severity of the diabetes or kidney disease.
Even if those goals are not met, despite correct treatment, you still benefit: every reduction in blood pressure leads to a reduction in the risk of cardiovascular disease.
How is high blood pressure treated?
 Treatment of high blood pressure always requires a lifestyle adjustment. If this is not sufficient, blood pressure lowering medicines are also prescribed.
Treatment of high blood pressure always requires a lifestyle adjustment. If this is not sufficient, blood pressure lowering medicines are also prescribed.
Non-drug: Lifestyle adjustment Lifestyle
adjustment is a first and essential step in the treatment of high blood pressure. All hypertension patients should improve their lifestyle without delay.
Depending on your blood pressure levels and the risk of cardiovascular disease, this may be the only treatment, or treatment with medicines will be started immediately or later.
The lifestyle recommendations largely correspond to the measures to prevent hypertension (see above):
- weight loss in case of overweight
- balanced dietary habits with particular attention to the high consumption of fruit and vegetables, lower salt consumption, less saturated fats, etc.
- more exercise (at least 30 minutes a day)
- moderating alcohol consumption
- do not smoke or stop smoking
- reducing stress.
If these recommendations are followed correctly, this can cause a significant reduction in blood pressure, sometimes as well as a reduction with the help of a medicine. The impact of these measures is like a sum total. This means that the application of various measures has an additional blood pressure lowering effect.
If medicines are still needed, these measures are better able to control blood pressure and usually require fewer medicines.
Blood pressure lowering drugs (antihypertensive drugs)
A healthy lifestyle is often not enough to lower blood pressure (sufficiently). Then blood pressure lowering drugs are also needed.
The choice of blood pressure lowering medicine(s) shall take into account, inter alia:
- other conditions (diabetes, cardiovascular diseases, kidney disease, asthma or COPD...)
- a previous heart or cerebral infarction (CVA)
- specific characteristics of the patient (such as age, race, etc.)
- the patient's previous experiences with antihypertensive drugs
- possible side effects, interactions and counter-indications
- pregnancy
- cost price
Step-by-step plan
One usually starts with one type of blood pressure lowering, for example a water pill (diuretic) or a calcium channel blocker. If the blood pressure does not fall sufficiently, one can add another blood pressure lowering agent, for example an ACE inhibitor, rather than increasing the dose of a drug. Increasing the dose usually has little effect on blood pressure, while the risk of side effects is increased. By combining different types of antihypertensive drugs in low doses, the side effects can be limited.
In case of a greatly elevated blood pressure, it may be considered to start combination therapy immediately.
It can take several weeks to months before the ideal combination of medicines is found.
Monthly monitoring of blood pressure is recommended until values return to normal and remain stable. After that, a quarterly or half-yearly check is sufficient.
More than one medicine
In most patients, two, sometimes three or more different medicines are needed to lower blood pressure sufficiently.
If possible, your doctor will prescribe a combination pill that combines multiple types of antihypertensive drugs, as this is easier and the chances of you forgetting a pill are smaller.
Lifelong
These medicines usually have to be taken for life. Medications have the best results if you take them as prescribed. Long-term use of medications is easier to maintain if you know what to expect from the drug. Therefore, ask your doctor how the medications work and what side effects the drug has. Also ask what side effects you should contact your doctor for. Never change the prescribed dose on your own initiative or stop treatment yourself.
If treatment is interrupted, blood pressure rises and complications may occur. It can even be dangerous to suddenly stop blood pressure lowering treatment: blood pressure can then rise rapidly and cause an acute complication (myocardial infarction, myocardial insufficiency, disorders in the cerebral blood vessels).
Research shows that about two out of three patients stop taking their medicines over time or take them irregularly. As a result, the blood pressure does not drop or does not drop sufficiently, with all the risks that entails.
Types of blood pressure lowering drugs
- Water pills or diuretics (especially thiazides and related)
These ensure that more salt and water are excreted through the urine. As a result, blood pressure drops. They are also likely to have a beneficial effect on elevated blood pressure through other, as yet unexplained mechanisms.
Water pills have relatively few side effects.
They are not recommended during pregnancy and in case of gout. - Calcium blockers or antagonists
These ensure that the muscles in the vascular wall contract less, causing the blood vessels to dilate and less calcium attaches to the inner wall of the arteries.
Possible side effects include.m headache, gastrointestinal complaints and thick ankles. - Inhibitors of the angiotensin conversion enzyme (ACE inhibitors)
These inhibit the conversion of the hormone angiotensin I into the artery-narrowing angiotensin II. This causes the arteries to dilate.
They are drugs with relatively few side effects. You can get itchy cough. They should not be used during pregnancy. - Angiotensin II antagonists ('sartans')
Block the action of the artery-constricting angiotensin II, while also preventing it from attaching to its receptors. This causes the arteries to dilate.
They have relatively few side effects. They should not be used during pregnancy. - Other blood pressure lowering medicines
There are other blood pressure lowering medicines that are used much less because they are less effective, have more side effects or are less well researched. They are usually used when the other agents do not work sufficiently, or sometimes in a hypertensive crisis.- Direct renin inhibitors (Aliskiren)
- Centrally acting antihypertensive drugs (clonidine, methyldopa, moxonidine
Methyldopa is mainly used in hypertension during pregnancy. - Vasodilators such as hydralazine and Urapidil are sometimes used in hypertensive crises and perioperative hypertension.
- Alpha blockers (Prazosin)